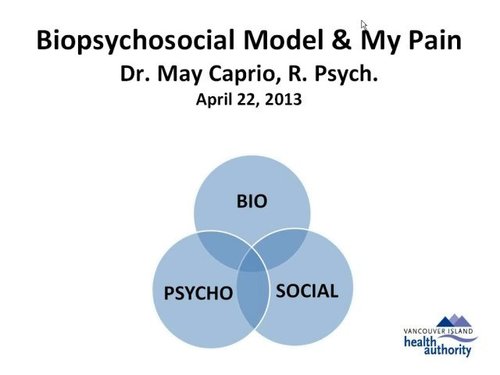
Chronic pain changes many things in life, most are invisible. Many people do not seem to understand chronic pain and its effects. Many people do not seem to understand that chronic pain sufferers have attempted numerous alternative therapies and know what therapies have worked or not worked for them. Some people have been misinformed or merely misunderstand.
In the spirit of informing those who wish to understand: These are some things that can help you to understand, and help, people who suffer from often debilitating, chronic pain.
- Remember that being sick does not mean that the sufferer is no longer a human being. Chronic pain sufferers spend the majority of their day in considerable pain. If one visits or lives with a chronic pain sufferer, the chronic pain sufferer may be unable to enjoy things they used to enjoy. The chronic pain sufferer remains aware, and desires to do what they used to perform. The chronic pain sufferer feels as if they are stuck inside a body they have little or no control. They want to enjoy work, family, friends, and leisure activities.
- Learn the code. Chronic pain sufferers will often talk differently from people free of constant pain. [1] A numeric pain scale is used as a quantitative measure for identification of intensity for pain so the doctors can measure effects of treatments. Description of pain on a scale measuring from 1 to 10, the 1 is “no pain at all, feel wonderful” and 10 is the “worst pain ever felt”. Do not assume the chronic pain sufferer is not experiencing pain when they say that they are fine. The chronic pain sufferer attempts to hide the pain due to lack of understanding in others. Accept that words may be inadequate to describe how the sufferer is feeling. Recall a time when you experienced pain, then multiply the intensity and attempt to imagine the pain present twenty-four hours everyday without relief. It’s hard to find the words for that sort of pain.
- Recognize the difference between “happiness” and “healthy”. When you have the flu, you probably have felt miserable. Chronic pain sufferers have experienced pain from 6 months to many years. Pain has caused them to adopt coping mechanisms that are not necessarily reflecting the real level of pain they feel. –
– Respect that the person who is in pain is trying their best. When the chronic pain sufferer says they are in pain – they are! They are merely coping; sounding happy and trying to look normal.- – Look for the signs of pain: grimacing, restlessness, irritability, mood swings, wringing of hands, moaning,sleep disturbance, teeth grinding, poor concentration, decreased activity, and perhaps even writing down suicidal thoughts or language.[2]
- Listen. The previous two steps made it clear that chronic pain sufferers can speak in code or make light of their pain than is the reality. The next best thing that you can do is to listen to them properly, and to make it clear that you both want to hear what they have to say and that you really have heard it. Use your listening skills to decode what they’re hiding or minimizing.
– Don’t be put off by the sufferer’s attempts at distracting you; be persistentListen. The previous two steps made it clear that chronic pain sufferers can speak in code or make light of their pain than is the reality. The next best thing that you can do is to listen to them properly, and to make it clear that you both want to hear what they have to say and that you really have heard it. Use your listening skills to decode what they’re hiding or minimizing. Read How to be a good listener for more details on being a great listener.- Understand and respect the chronic pain sufferer’s physical limitations. Being able to stand up for ten minutes doesn’t necessarily mean that the sufferer can stand up for twenty minutes, or an hour, or give you a repeat performance whenever. Just because the person managed to stand up for thirty minutes yesterday doesn’t imply that they will be able to do the same today. With a lot of diseases, a person may exhibit obvious signs of immobility, such as paralysis, or total immobilization due to weakness, etc. With chronic pain however, it is confusing to both the sufferer and the onlooker, and their ability to cope with movement can be like a yo-yo. The sufferer may not know, from day-to-day, how they are going to feel when they wake up and each day has to be taken as it comes. In many cases, they don’t know from minute to minute. That is one of the hardest and most frustrating components of chronic pain.
Continue on www.wikihow.com
Blessings,
Jacqui